While surgical mesh has been successfully used in hernia repairs since WWII, 3D printing of prosthetic medical devices has so far focused on items like hearing aids, dental crowns, and limb prosthetics designed to replace or support bones and other rigid parts of the body. These devices are often printed from solid, relatively inflexible materials.
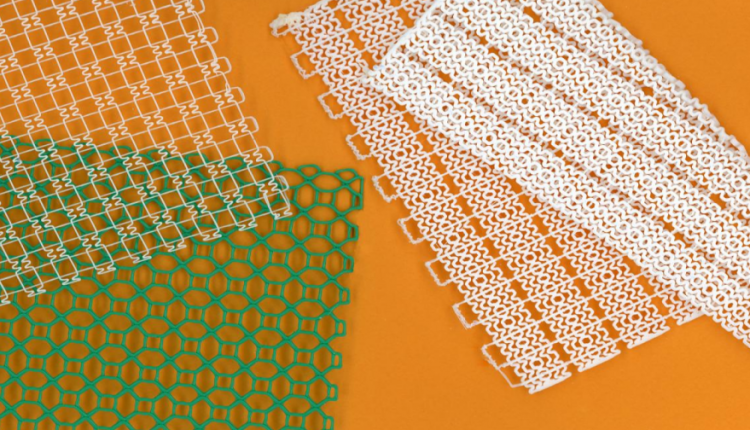
But MIT engineers have recently designed pliable, 3D-printed mesh materials whose flexibility and toughness can be fine-tuned to emulate and support softer tissues such as muscles and tendons. They can tailor the intricate structures in each mesh, and see the tough yet stretchy fabric-like material being used as personalized, wearable supports, including ankle or knee braces or even implantable devices, such as hernia meshes, that better match to a person’s body.
As a demonstration, the team printed a flexible mesh for use in an ankle brace. They tailored the mesh’s structure to prevent the ankle from turning inward—a common cause of injury—while allowing the joint to move freely in other directions. The researchers also fabricated a knee brace design that could conform to the knee even as it bends and produced a glove with a 3D-printed mesh sewn into its top surface, which conforms to a wearer’s knuckles and provides resistance against involuntary clenching that can occur following a stroke.
“This work is new in that it focuses on the mechanical properties and geometries required to support soft tissues,” says Sebastian Pattinson, who conducted the research as a postdoc at MIT and is now at Cambridge University. “3D-printed clothing and devices tend to be very bulky,” Pattinson says. “We were trying to think of how we can make 3D-printed constructs more flexible and comfortable, like textiles and fabrics.”
Inspired by collagen
Pattinson found further inspiration in collagen, the structural protein that makes up much of the body’s soft tissues and is found in ligaments, tendons, and muscles. Under a microscope, collagen can resemble curvy, intertwined strands, similar to loosely braided elastic ribbons. When stretched, this collagen initially does so easily, as the kinks in its structure straighten out. But once taut, the strands are harder to extend.
Pattinson designed wavy collagen-emulating patterns, which he 3D-printed using thermoplastic polyurethane as the printing material. He then fabricated a mesh configuration to resemble stretchy yet tough, pliable fabric. The taller he designed the waves, the more the mesh could be stretched at low strain before becoming stiffer—a design principle that can help to tailor a mesh’s degree of flexibility and helped it to mimic soft tissue.
The researchers printed a long strip of the mesh and tested its support on the ankles of several healthy volunteers. For each volunteer, the team adhered a strip along the length of the outside of the ankle, in an orientation that they predicted would support the ankle if it turned inward. They then put each volunteer’s ankle into an ankle stiffness measurement robot or Anklebot. The Anklebot moved its ankle in 12 different directions, and then measured the force the ankle exerted with each movement, with the mesh and without it, to understand how the mesh affected the ankle’s stiffness in different directions.
In general, they found the mesh increased the ankle’s stiffness during inversion while leaving it relatively unaffected as it moved in other directions.
A simple, versatile solution, the mesh can be made on a basic desktop 3D printer, and its mechanics precisely tailored to match soft tissue.
The team’s ankle brace was made using relatively stretchy material. But for other applications, such as implantable hernia meshes, it might be useful to include a stiffer but equally conformable material. So they developed a way to incorporate stronger and stiffer fibers and threads into a pliable mesh, by printing stainless steel fibers over regions of an elastic mesh where stiffer properties would be needed, then printing a third elastic layer over the steel to sandwich the stiffer thread into the mesh.
The combination of stiff and elastic materials can give a mesh the ability to stretch easily up to a point, after which it starts to stiffen, providing stronger support to prevent, for instance, a muscle from overstraining.
The team also developed two other techniques to give the printed mesh an almost fabric-like quality so it could conform easily to the body in motion. Textiles are flexible because their fibers move easily relative to each other, and mimicking that capability was an important aspect of the project.
In traditional 3D printing, material is printed through a heated nozzle, layer by layer. When the heated polymer is extruded it bonds with the layer underneath it. Pattinson found that, once he printed the first layer, if he raised the print nozzle slightly, the material coming out of the nozzle would take a bit longer to land on the layer below, giving the material time to cool. As a result, it would be less sticky. By printing a mesh pattern in this way, Pattinson was able to create layers that were free to move relative to each other rather than being fully bonded to each other and developed a multilayer mesh that draped over and conformed to the shape of a golf ball.
Finally, the team designed meshes that incorporated auxetic structures—patterns that become wider when you pull on them. For instance, they were able to print meshes, the middle of which consisted of structures that, when stretched, became wider rather than contracting as a normal mesh would. This property is useful for supporting highly curved surfaces of the body. To that end, the researchers fashioned an auxetic mesh into a potential knee brace design and found that it conformed to the joint.
“There’s potential to make all sorts of devices that interface with the human body,” Pattinson says. Surgical meshes, orthoses, even cardiovascular devices like stents— you can imagine all potential benefits from the kinds of structures we show.”
Source: MIT